
Table of Contents
Origins Of IBS Symptoms
Controlling Diarrhoea In The Short Term
Gut Bacterial Imbalances And IBS
Can Antibiotics Kill Off The Bad Bugs?
Healthy Balanced Diet
Probiotics And Medication vs Elimination Diets
After Probiotics And Medication
Probiotics Don’t Work Or Partially, What Next?
Tried Everything But Still Have Issues
What Does A Good Microbiome Look Like?
What Do Good Microbes Do For You?
Free Microbiome Course
Further Reading And References
Origins Of IBS Symptoms
Some factors may make someone more prone to IBS:
- Physiological. For example, someone born with an extra long, loopy colon may experience IBS-C (constipation dominant IBS) type symptoms. This is because stool has a longer to travel, meaning that there is more time for the body to extract water from stools, making them hard and more difficult to pass
- Psychological. For instance, genetically being a highly sensitive person (HSP) may have links with IBS (12) (11)
- Early life experience. Women with severe functional gastrointestinal disorders including IBS often have a history of sexual and/or emotional abuse. This is as high as 30% in those attending gastroenterology clinics. Trauma from abuse can cause changes in brain chemistry which can impact gut motility as well as distort pain recognition. These changes include (14):
- relatively higher levels of norepinephrine (noradrenaline) which may lead to a state of hyperarousal or hypervigilance
- relatively lower levels of serotonin which regulates mood
- dysregulation of the hypothalamic-pituitary-adrenal (HPA) system which controls reactions to stress
- Current social stresses
It is often combination of psychological factors and sensitisation of the gut after infection that can trigger irritable bowel syndrome in adults.
In fact, whilst the majority of patients suffering from gastroenteritis (the infection and inflammation of the digestive system) recover, 10% will develop IBS symptoms. (17)
Additionally, a predisposition to IBS may be inherited. From a study, 6 genes have been associated with IBS, involving CKAP2/TPTE2P3, NCAM1, DOCK9, CADM2, BAG6, and PHF2/FAM120A. Interestingly, NCAM1, DOCK9, CADM2, and PHF2/FAM120A from the list have associations with anxiety disorders. (20)
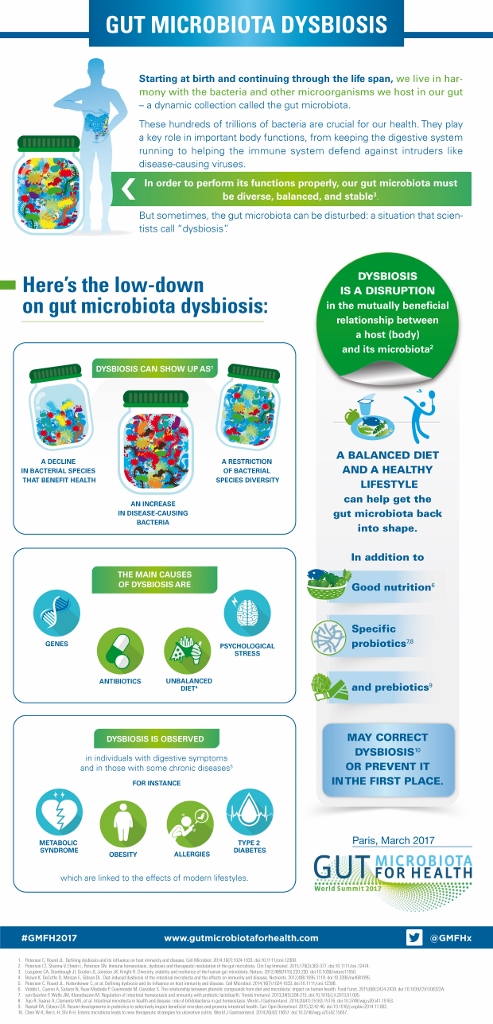
The below infographic from Gut Microbiota For Health, provides a good explanation regarding how the gut microbiome can become imbalanced leading to what is known as gut microbiota dysbiosis where bad bugs can dominate in the gut, which can contribute to IBS symptoms in some people:
Controlling Diarrhoea In The Short Term
If you need to quickly bring diarrhoea under control since it affecting your ability to lead a normal life or even leave the house etc., there is of course Imodium (Loperamide), but there are also dietary measures. You can try just consuming white Jasmine rice alone or white Jasmine rice with some easily digestible protein for a day or two. This will provide energy and will be only digested in the small intestine with no residue going to the colon to give your colon a rest. Once things are starting to get under control you could add in some easily digested vegetables such as cooked carrots. Once you start to become constipated you can gradually resume your normal diet. People often have plain white toast with diarrhoea, however, wheat in the bread contains fructans (a FODMAP) which might be more of a challenge for your digestive system if it is feeling particularly sensitive.
Gut Bacterial Imbalances And IBS
The gut microbiome refers to the microorganisms that live in your gut (2). A baby’s gut microbiome is shaped from the flora that the baby comes into contact with during the birthing process, either from the mother during a natural delivery or from skin or bacteria found in hospitals during caesarean section. (18) Interestingly, though, the environment, diet, antibiotics, and genes have a more relevant influence in crafting your microbiome than that provided during the birthing process. (19)
From the infographic further above it can be seen that these microorganisms play a number of roles in your overall health. In some people with IBS, a gut bacterial imbalance, whereby a person’s bad gut bugs have the upper hand over good (a state of dysbiosis as described above) can cause symptoms such as excess gas, pain or disordered bowel movements. These imbalances can additionally create food intolerances. There are certain types of carbohydrates called FODMAPs, which are not absorbed very well and their residue can end up in the colon. This residue feeds gut bacteria in the colon. Ordinarily feeding gut bacteria is a really good thing. When you feed good gut bacteria these produce by-products that have great health effects in the gut and throughout the body. However, when there is an overgrowth of bad bugs, these bugs are fed too which helps to keep them established and cause symptoms. If you investigated the bacteria in a person’s gut, it would contain both good and bad bugs. This is not a cause for concern. The issue is when the good bugs are not keeping the bad bugs under control and they are in numbers that cause symptoms (3). Note that FODMAPs are not a cause of IBS, but are food components that can aggravate underlying IBS related to an “exaggerated bowel response to gaseous distension” (15)
Can Antibiotics Kill Off The Bad Bugs?
The problem with antibiotics is that they can kill both good bugs and bad bugs in the gut. Antibiotics can also be culprits in creating these gut imbalances in the first instance potentially leading to IBS (see infographic above). Furthermore, after a course of antibiotics your gut microbiome may return to its original state after a while, including allowing bad bugs to remain (4). Having said that, if you have an infection for which your doctor recommends antibiotics since the infection could impact your health, you are best advised to go with that recommendation.
Healthy Balanced Diet
If you have been diagnosed with IBS by a qualified GP, the official recommendation is to ensure that you are eating a healthy balanced diet first, including a variety of fruits, vegetables and cereal fibres. A good example of a healthy balanced diet is the Mediterranean diet.
Sometimes poor eating can trigger IBS symptoms. If your gut microbiome isn’t nourished properly, bad bugs may be more likely to take hold and cause symptoms. If you are eating a healthy balanced diet and still experiencing symptoms, the next step is to try a good probiotic.
Probiotics And Medication vs Elimination Diets
The right probiotic, which contains good gut bacteria, may be able to shift the balance in the gut to help defeat the bad bugs and reduce symptoms without the potential detrimental effects of antibiotics. Some medical professionals recommend starting with the FODMAP elimination and reintroduction diet. This is to help find out which types of FODMAPs or specific foods lead to symptoms and then eliminate them from the diet. However, since foods containing FODMAPs are good for you, I would not recommend starting with the FODMAP elimination and reintroduction diet. If you can find a good probiotic that reduces symptoms, it may be unnecessary to perform an elimination and reintroduction diet, allowing you to continue to eat these foods that are good for your health. Alternatively, probiotics may make you tolerant to a wider range of foods, which means that if you do need to carry out elimination and reintroduction of foods, you may find that there are more FODMAPs that you can reintroduce into your diet, than if you hadn’t tried probiotics. I have tried many probiotics over the years, but the one that has worked for me the best and has been scientifically studied for IBS is Alflorex which contains 35624 Bacteria Culture [Bifidobacterium Longum]. It contains a particularly strong strain of good bacteria which is normally passed from mother to baby during a natural birth to prime the baby’s gut defences, so it is particularly strong strain and good at fighting infections caused by an overgrowth of bad bacteria. It can take a 3 month trial to see full benefits of taking Alflorex in some people. Note that I have no commercial affiliation with the producers of Alflorex.
Plus, you may need medication to help your symptoms and to improve food intolerance – for example for diarrhoea with or without cramping there is mebeverine (Colofac) or Buscopan and enteric coated peppermint may help with pain. For instance, whilst you are trialling a probiotic, you may need additional support from these, including Imodium (Loperamide) if mebeverine (Colofac) or Buscopan are not strong enough for your diarrhoea symptoms.
After Probiotics And Medication
If you have managed to achieve an improvement in symptoms from probiotics and medication (if needed), it is necessary to have as a diverse a diet as possible, such as that from the Mediterranean diet, eating a wide variety of fruits and vegetables with different colours, whole grains, pulses, nuts, seeds, healthy oils such as olive oil and lean meats to encourage a large range of different types of good bacteria to grow in the gut (bacterial diversity). Data from the American Gut Project has revealed that consuming more than 30 different plant-based foods on a weekly basis is associated with a widely diverse gut microbiota (5) (6). It is this bacterial diversity that will help to guard against pathogens and hence IBS symptoms in future. Once the gut becomes more balanced and you are feeding your good gut bacteria well through your diet, it may be possible to stop taking probiotic supplements or to cut back the frequency that you take them.
This is also a good time to introduce prebiotic foods or prebiotic supplements to further nourish a healthy microbiome to help maintain it.
Probiotics Don’t Work Or Partially, What Next?
If you have tried a variety of probiotics that have some good evidence for them and nothing has changed, it is possible that you don’t have a gut bacterial imbalance, there are other factors affecting your IBS or you haven’t managed to hit upon the the specific bacterial strains that your body needs. Unfortunately, the research in this area is not complete. You could, try the FODMAP elimination and reintroduction diet, to find out if there are specific foods that are causing you issues. This can also be tried if you have received some symptom improvement from probiotics and medication (if needed) and want to continue with these, but also you would like to uncover any remaining food intolerances. Since there currently isn’t a cure for IBS, this situation is more likely to be the case. However, as previously mentioned FODMAPs are good for you so ideally you want to eat as many as you can tolerate. This diet is best conducted under the guidance of a NHS dietitian from a referral from your GP.
Tried Everything But Still Have Issues
If you are still experiencing issues after trying probiotics, medication (if needed) and the FODMAP elimination and reintroduction diet and you still have frequent diarrhoea, you could ask your GP for a test for Bile Acid Malabsorption (BAM). There is a separate test and treatment for that (7). In rare cases you may be suffering from SIBO (small intestinal bacterial overgrowth). Unfortunately the tests for SIBO aren’t accurate and this can be a tricky area. Please see separate menu option on this (here). There is also gastroparesis that can have some of the symptoms of IBS, but not others – see here.
What Does A Good Microbiome Look Like?
Scientists are unable to provide a specification for a healthy microbiome including whether specific organisms are present or absent. This would be highly dependent on a number of factors such as age ranges and individual populations. Equally they are unable to define an unhealthy microbiome since it is normal for the microbiome to consist of both pathogenic (bad) and friendly (good) gut bacteria in healthy individuals. (8)
However, there may be some features of an altered gut microbiome which include:
- Low total number of bacterial specifies in the gut (microbiota richness)
- Low amount of individual bacteria from each bacterial species in the gut (microbiota diversity)
- Reduction of short chain fatty acid-producing bacteria
- Instability in composition of the microbiome over time
There are commercial microbiome testing facilities on the market. This involves analysis of faecal samples. Microbes that culture easily in a test setting is not representative of a person’s microbiome as a whole, since this is predisposed to bacteria that like oxygen such as pathogens (bad bacteria) whilst good bacteria could be missed as they grow without oxygen. There are emerging technologies that help overcome this type of culture based testing. The other type of testing involves the analysis of DNA in stool samples. More used in research are tests involved in studying the by-products (metabolites) of bacteria, but these are relatively unknown and provide no value as health markers at this stage.
Microbiome testing is still in early stages. Studying the microbiome of stool does not reflect the changing nature of microbiome found in the gut and the variation found in different parts of the gut. Finding ‘bad bacteria’ in the gut is normal and a specific species may or may not be contributing to someone’s symptoms. There is still so much more to be found out about gut bacteria. Around 20% of bacterial DNA and over 40% of of the 10 million microbial genes’ functions have not been identified. This means that the science is not there yet in terms of correcting specific by-products of bacteria either through diet or supplements. Current microbiome testing has limited value in guiding treatments. Treatments at this stage are better guided by symptom severity.
There is some early research that uses the microbiome to identify responders and non responders to dietary interventions in IBS patients.
The current commercial microbiome tests available are ahead of their time in terms of having any real use for the consumer.
If a microbiome imbalance is suspected with dominant bad bugs causing symptoms, which often happens with IBS, it would be far more appropriate and far cheaper to try a trial of a good probiotic to shift the balance than spending inordinate sums on microbiome testing. Even if bad bugs are found during testing (which is normal) and the decision is to take antibiotics or antimicrobials to try to remove them, these not only act on the bad bugs, but also compromise the good bacteria in the gut, which are meant to keep the bad bacteria under control. Additionally, it is normal for bacteria to grow back after antibiotic treatment, including the bad bugs, rendering the process futile. It is only in cases of severe infection from, for example, clostridium difficile that antibiotics may be needed, but this should always be under the guidance from the GP and related to tests that they run and not from commercial testing companies.
There are some stool tests that measure stool fat (to assess for fat malabsorption) or stool elastase (a marker for adequate pancreatic enzyme production), but these are available through your health care provider and there is no need to pay huge sums for commercial tests. (16)
What Do Good Microbes Do For You?
A healthy microbiome mainly consists of the following groups of gut bacteria: Firmicutes and Bacteroidetes followed by Actinobacteria and Verrucomicrobia. The sub-groups of bacteria that make up these can be found in their aforementioned links.
The bacterial species occurring in the gut microbiota include: Gemella spp., Megasphaera spp., Pseudomonas spp., Prevotella spp., Streptococcus spp., Rothia spp., Veillonella spp., Clostridium spp., Porphyromonas spp., Eubacterium spp., Ruminococcus spp., Enterobacter spp., Enterococcus spp., Lactobacillus spp., Peptostreptococcus spp., Fusobacteria spp., Lachnospira spp., Roseburia spp., Butyrivibrio spp., Faecalibacterium spp., Proteobacteria spp.
These bacteria are normally helpful and provide a number of functions including:
- fermentation of carbohydrates to metabolise nutrients from them
- being involved in the digestion, absorption of nutrients, fluids and electrolytes from food
- ferment fibre to the compounds that intestinal bacteria feed on
- production of butyrate, a short chain fatty acid (SCFA) and by-product of the aforementioned fermentation, which is an important energy source for the cells that make up the surface of the colon and have anti-inflammatory and anticancer properties
- assist with the breakdown of fats (lipids)
- enhance metabolism of proteins
- key in synthesising vitamin K, B12, biotin and conjugated linoleic acids (CLA – a fatty acid found in meat and dairy)
- conversion of bile acids into other components
- involved in the breakdown of various polyphenols (healthful micronutrients from plants)
- maintain the integrity of the gut barrier and structure of the gastrointestinal tract, due to substances produced by Bacteroides thetaiotaomicron, Lactobacillus rhamnosus GG and Akkermansia muciniphila
- contributes to the structural development of the gut mucosa (inner lining of the gut)
- makes up part of the the gut barrier which also consists of gut surface cells (epithelium) and immune cells and helps to protect against toxins and pathogens from the external environment, in addition to secreting antibodies and participating in the transmission of signals to other cells and organs
Free Microbiome Course
I can highly recommend this free course if you would like to understand more about the microbiome – link here (10).
Further Reading And References
(1) GMFH Editing Team: Gut Microbiota Dysbiosis, Gut Microbiota for Health, April 1st, 2017
(2) Gut Microbiota for Health: Gut microbiota info
(7) NICE : Bile acid malabsorption: colesevelam